June, 2025 6 MIN READ
Let’s Discuss Breast and Cervical Cancer for the LGBTQIA+ Community
Everyone has breast tissue and people of all genders can get breast cancer, and there are a few myths in the LGBTQIA+ community around cervical cancer. This Pride Month, Boux Avenue spoke with CoppaFeel!, the first youth-focused breast health awareness charity, and The Eve Appeal, a gynecological cancers charity, to help offer awareness, debunk myths, and help you feel more confident about checking your chest, attending your cervical screening, or both.
Things to Know About Breast Cancer:
Breast cancer can affect any body
CoppaFeel!’s message is for everyone, because everyone has breast tissue. Breast cancer can affect anybody, no matter your age or gender, so it’s really important to get to know what’s normal for your body—especially at times when your chest may experience changes, like around your period for those who menstruate, during pregnancy, or during transition.
CoppaFeel!’s resources for trans and non-binary people
To make sure all young people are empowered with the information they need to get to know their bodies, CoppaFeel! has worked with the amazing cancer support and advocacy charity for the LGBTIQ+ community, Outpatients, to create resources and advice for trans and non-binary people. You can download these here.
Checking your chest - top tips
Together they also established these three handy tips when it comes to getting to know your chest.
- Check regularly — If dysphoria is making this difficult, try different methods, positions, or settings, like checking without a mirror, beneath loose clothing, or on days when you feel less dysphoric.
- Look and feel — Check all parts of your chest, including your armpits, up to your collarbones, and your nipples. If you have developed breasts as part of your transition or have implants (or plan to get them), it’s still important to get to know your new normal.
- If in doubt, get checked out — Even if you have had top surgery, some tissue usually remains around the nipple, under the collarbone, and in the armpit that needs to be checked. Early detection improves treatment and survival rates.
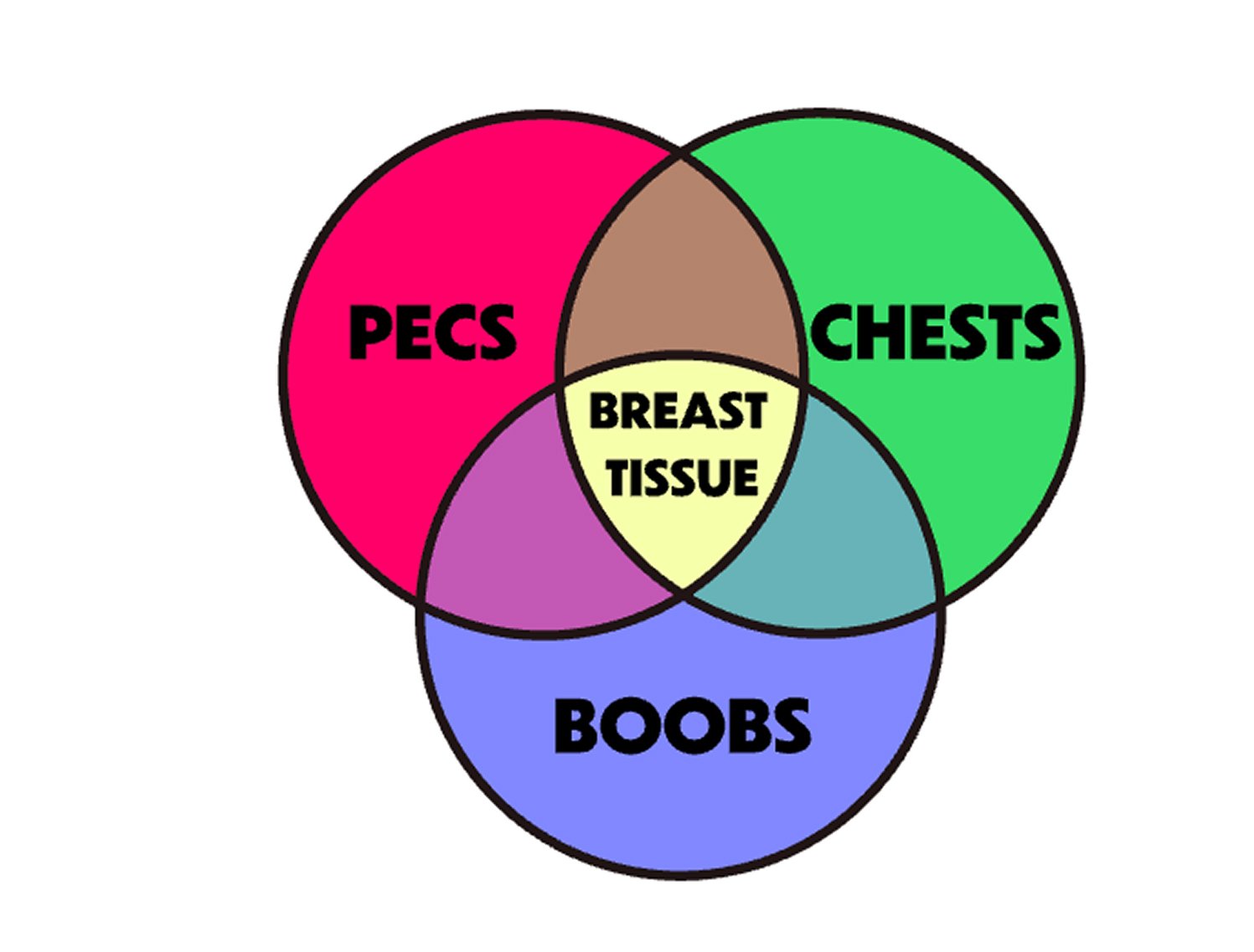
What do you call your chest?
It’s really important that messaging around checking is as inclusive as possible. That’s why CoppaFeel! use lots of terms to describe your chest area. Did you know CoppaFeel!’s digital tool, The Self Checkout, has a special feature where you can choose the terms you would like to use to refer to your chest/boobs/pecs/breasts? Whatever you prefer to call them is good with us, we just want you to get checking them!
CoppaFeel! advocates that there isn’t one specific way to check; you should do so in a way that feels comfortable for you. With this in mind, the charity encourages their amazing community to share #HowICoppaFeel, and you can check out some of that fab content on Instagram here.
Getting To Know What’s Normal for Your Chest
The signs may look different on your skin tone or your body. It’s really important to know what’s normal for you.
Things to know about Cervical Screenings
We understand that cervical screening appointments can be difficult for some people, and that if you are part of the LGBTQ+ community there are additional barriers that might prevent you from having your test. However, it is important to get screened if you can.
If you have any worries or concerns about cervical screening speak to your GP. The Eve Appeal’s Ask Eve nurse service can also give free advice.
Going for your cervical screening: Top Tips
Anyone with a cervix is at risk of developing cervical cancer. If you are a trans man, are transmasculine, or a non-binary person who has a cervix (if you haven’t had a total hysterectomy which removes the womb and cervix), we understand that attending a cervical screening appointment may be emotionally and physically difficult for you.
It can be helpful to have a separate appointment with your nurse or doctor beforehand and talk through the process with them. We also have created a list of tips to help prepare you for your screening:
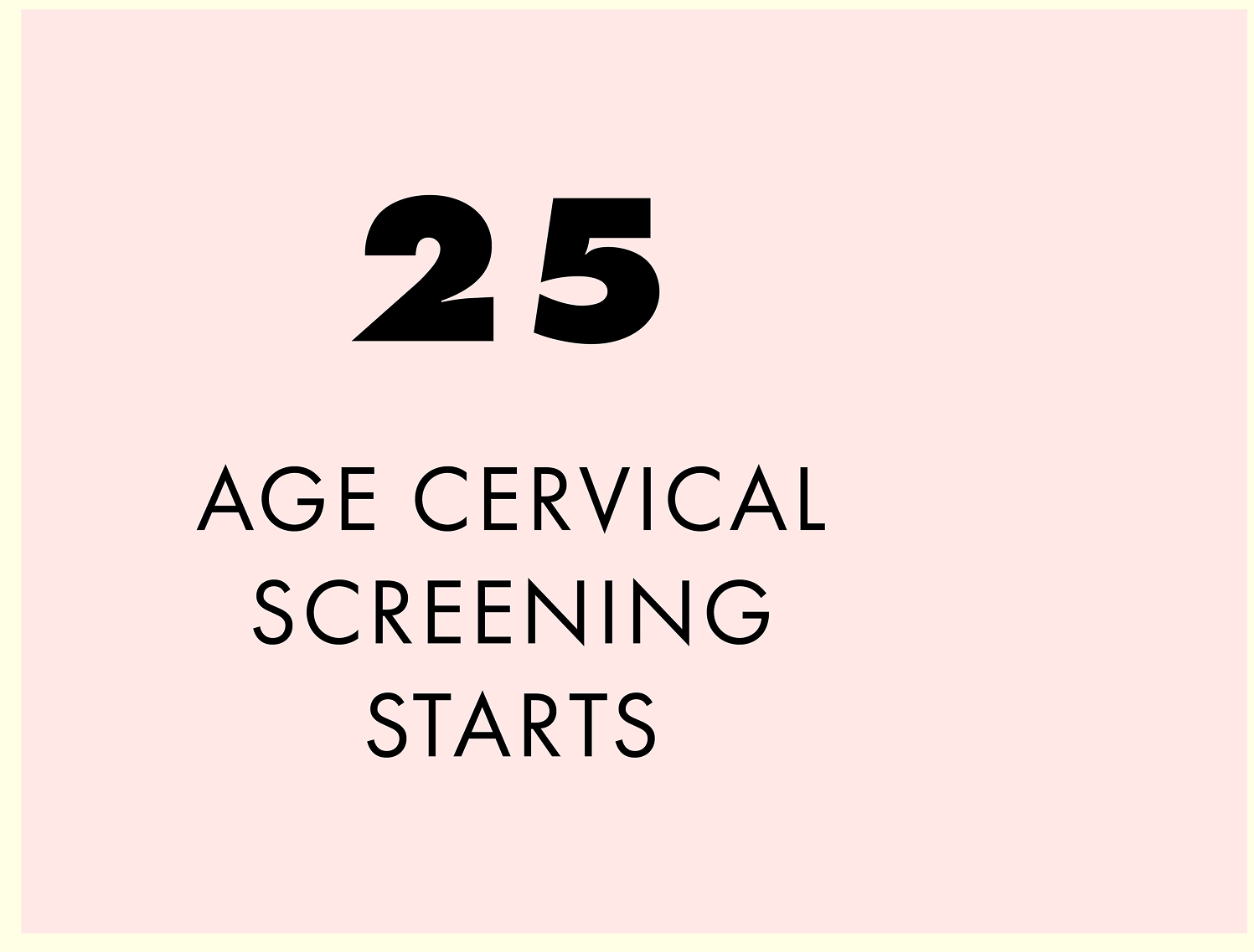
Get booked in:
If you’re registered as male at your GP surgery, you may not receive an invitation letter to go for your cervical screening. If you are 25 or over and have a cervix, you can call your GP to find out if you are due and get an appointment booked. You can also opt in to get automatically invited in the future. You can also be screened at some local sexual health services if you prefer.
Relaxation is key:
As humans, when we hear the words ‘just relax’, we often do the exact opposite! But try to relax in whatever way you can. What normally relaxes you? Whether it’s playing your favourite music or having a friend or partner with you for support, use these tools to help you during your screening. Whatever you can do to try and feel as calm as possible..
Lubricate:
If you are post menopausal or taking testosterone, you will have less natural lubrication, which can make a cervical screening test more uncomfortable. Try using a vaginal moisturiser,which is different from a lubricant, for three weeks before your appointment to make inserting a speculum easier and more comfortable. You will need to stop using this two days before your test. Your GP or nurse can prescribe an oestrogen cream or pessary for you to start using three weeks before your cervical screening. You should use this for two weeks and stop one week before your test. This will reduce your vaginal dryness and make your screening more comfortable. It is safe to use as it only works on the vaginal tissues to increase lubrication and is not absorbed into the body, so will not affect gender affirming care.
Anxiety about going for a cervical screening
Cervical screening can be daunting. There isn’t much information out there if you are trans, non-binary or intersex.There is no pressure to have your screening test done on your first appointment. Sometimes multiple appointments are needed so that trust is built up between you and your nurse or doctor.
If you are finding your screening difficult for whatever reason, it’s absolutely fine to need extra time or another appointment in order to feel ready and prepared. Remember that the nurse doing the cervical screening is there to support you and make the test as comfortable as possible.
You may encounter health care professionals who lack knowledge of trans, non-binary, and intersex identities. This can make discussing your needs more difficult or result in a bad experience. If there is one nearby, you may feel more comfortable attending a trans specific clinic.
Cervical screening frequently asked questions
Breast cancer can affect any body
CoppaFeel!’s message is for everyone, because everyone has breast tissue. Breast cancer can affect anybody, no matter your age or gender, so it’s really important to get to know what’s normal for your body—especially at times when your chest may experience changes, like around your period for those who menstruate, during pregnancy, or during transition.
CoppaFeel!’s resources for trans and non-binary people
To make sure all young people are empowered with the information they need to get to know their bodies, CoppaFeel! has worked with the amazing cancer support and advocacy charity for the LGBTIQ+ community, Outpatients, to create resources and advice for trans and non-binary people. You can download these here.
Breast cancer can affect any body
CoppaFeel!’s message is for everyone, because everyone has breast tissue. Breast cancer can affect anybody, no matter your age or gender, so it’s really important to get to know what’s normal for your body—especially at times when your chest may experience changes, like around your period for those who menstruate, during pregnancy, or during transition.